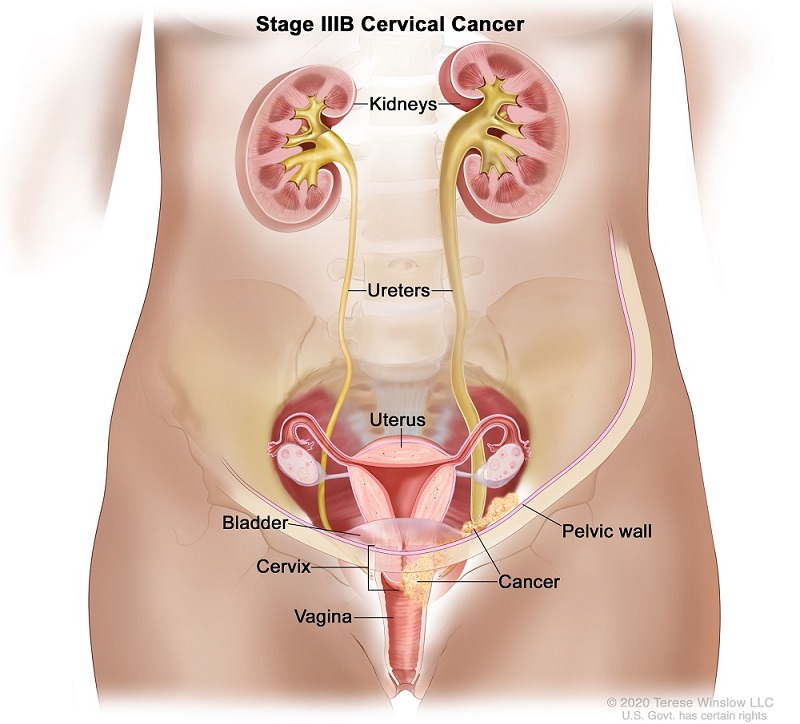
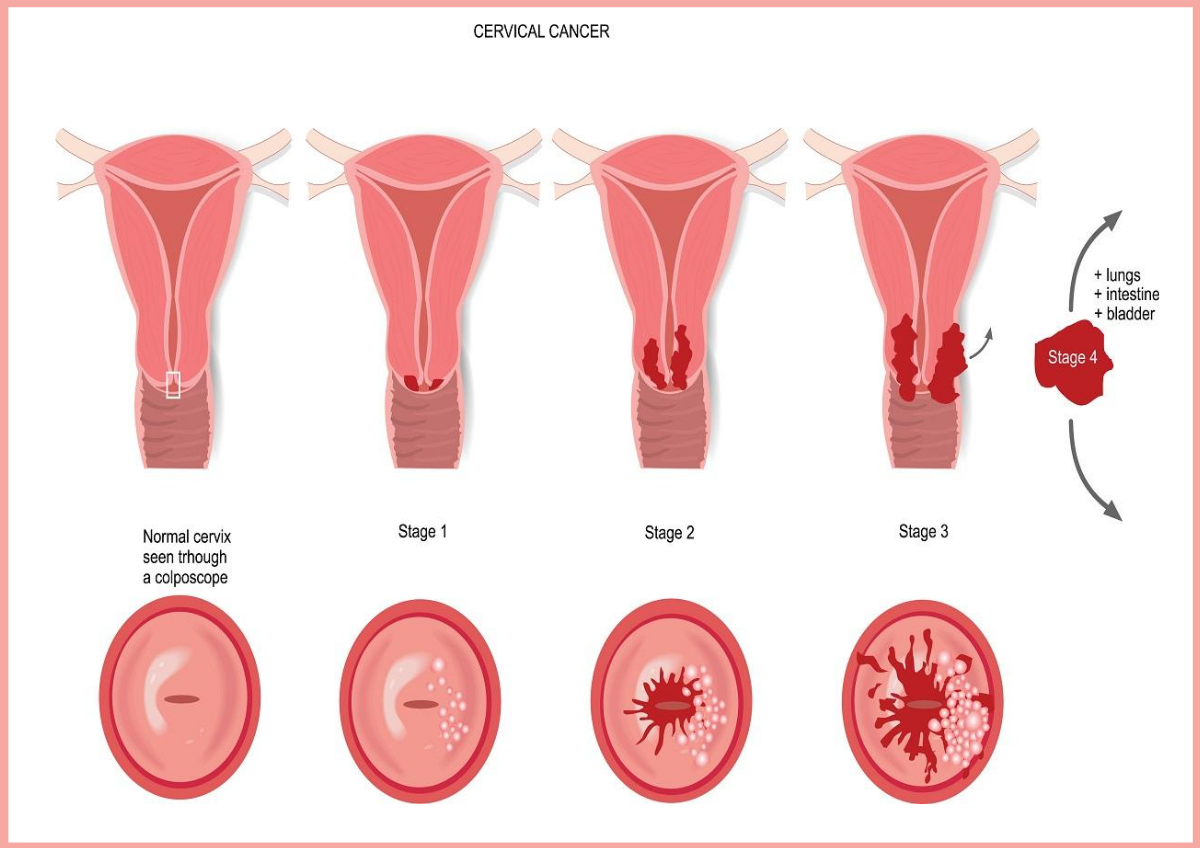
Cervical cancer is a type of cancer that occurs in the cells of the cervix (the entrance to the womb from the vagina). It usually affects sexually active women aged between 30 and 45.
Most cases of cervical cancer are caused by different strains of the HPV (human papillomavirus). HPV is a sexually transmitted infection that can be passed on through any type of sexual contact with a man or a woman.
There are more than 100 types of HPV, many of which are harmless. When someone’s body is exposed to HPV, the body’s immune system typically prevents the virus from doing harm and may lay dormant and even disappear after a while. But some types can survive for years causing abnormal changes to the cells of the cervix, which can eventually lead to cervical cancer.
Two strains, HPV 16 and HPV 18, are known to be responsible for most cases of cervical cancer.
You can reduce your risk of developing cervical cancer by having a smear test and receiving the HPV vaccine.
The transformation zone is the area where cells are most likely to turn cancerous and this is the area that is tested during a pap smear.
Types of Cervical cancer
Knowing the type of cervical cancer one has will determine the treatment to use.
Squamous cell carcinoma
This type starts from the squamous cells (flat, skin cells ) that line the ectocervix. The Ectocervix is the outer part of the cervix leading down into the vagina. The majority of cervical cancers fall into this category.
Adenocarcinoma
This type starts from the glandular cells (column shaped cells ) that line the endocervix, which leads up to the womb. This is the second most common type of cervical cancer.
Adenosquamous carcinoma
This type of cancer have both squamous and glandular cancer cells.
Risk factors/causes of Cervical cancer
-
HPV:
This is the leading cause of most cervical cancers. HPV is a sexual transmitted infection which is quite common and clears off the immune system on its own within 2 years for some people. However, some people’s immune system are unable to fight off the infection and some strains may lead to cervical cancer. The two types of HPV strains most known to cause cervical cancer are HPV 16 and 18.
-
Sex
Having sex at an early age and having more sexual partners will increase your risk of having HPV which can lead to cervical cancer.
-
Smoking
Smoking can increase your risk of cervical cancer and is linked to squamous cells cervical cancer.
-
Weakened immune system
If your immune system is weakened as a result of another health condition and you have HPV, then you are at greater risk of developing Cervical cancer