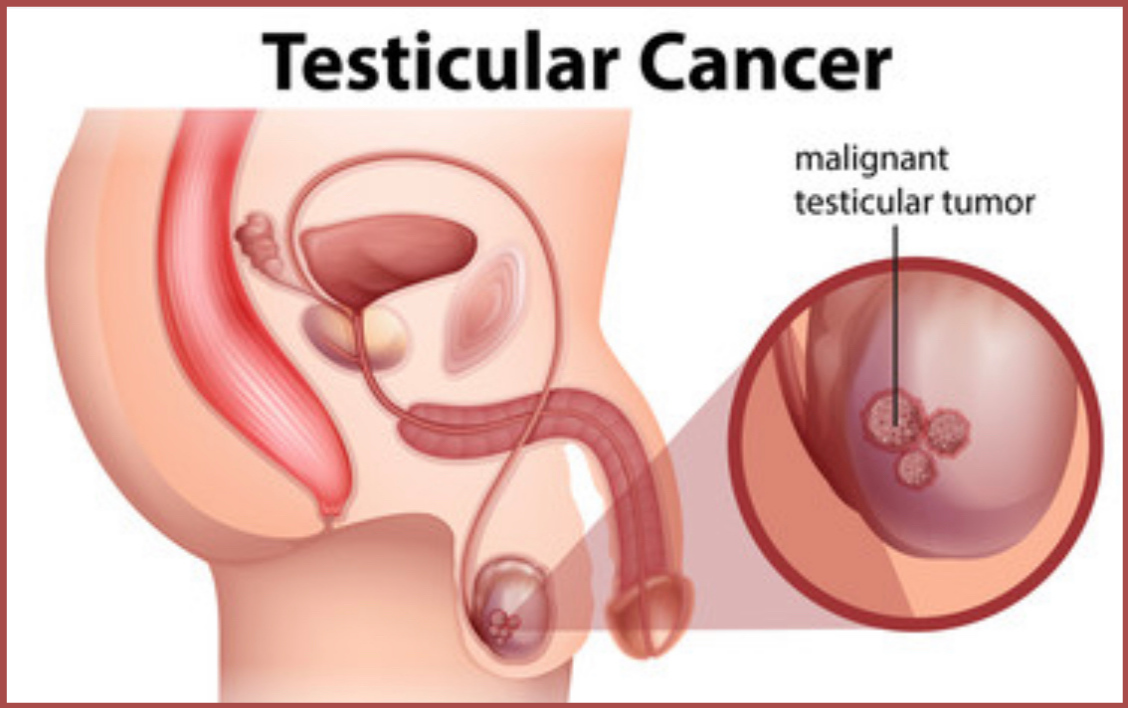
The testes, which are part of the male reproductive system, make the male sex hormones and produce sperm. This type of cancer starts in the testes which are located in the scrotum ( a loose bag of skin that is present under the penis)
One of the positive points of this type of cancer is that it is easily treatable even if it has spread outside the testicles. However, in such cases, there may be a combination of treatments.
Testicular cancer is the most common cancer that affects the male population. It mostly affects individuals between 15 to 44 years of age, and is less common as they get older According to research, testicular cancer affects Asians, African, and Central Americans the least. This research is in comparison to the European populations. Africa has the lowest rate of incidence among all the other continents i.e., 0.3 to 0.6.
Types of Testicular cancer
Testicles compose a complex network of cellular structures. These contain different types of cells; each type of these cells can develop into a type of cancer. The importance of knowing the type of cells helps to find out the type of cancer. This also improves the treatment and outlook of the disease.
Germ Cell Tumours
The majority of testicular cancers are tumours in the germ cells. These constitute 90% of such types of cancers. Germs cells help in the production of sperms. Seminomas and Non-seminomas are the two types of germ cell tumours. Both of these can occur in combination or individually.
Seminomas
Seminomas can grow and spread but spread at a slower rate than seminomas. It also has further two subtypes;
Classical seminoma that constitutes 95% of the cases. It affects men between the age of 25 to 45 years. The other type is spermatocytic seminoma. This rare type of seminoma affects older men. It grows slowly and is less likely to spread to other parts.
Non-Seminoma
This type of non-seminomas affects men in their late teens and early thirty’s. There are four types of non-seminomas. The majority of these types can exist in a combination of different types. However, it does not affect the course of treatment.
Embryonal Carcinoma involves 40% of testicular cancers. The name is because cells of this tumour look like embryos microscopically. Yolk Sac Carcinoma is the second type of Non-seminoma. This is because the cells resemble yolk sacs under the microscope. Choriocarcinoma, the third type of tumour is an aggressive form of the tumour. It affects adults. It can even spread to various other parts of the body.
The last sub-type is a teratoma. It contains three layers that resemble a developing embryo. Teratoma also has three further subtypes.
Symptoms of Testicular cancer
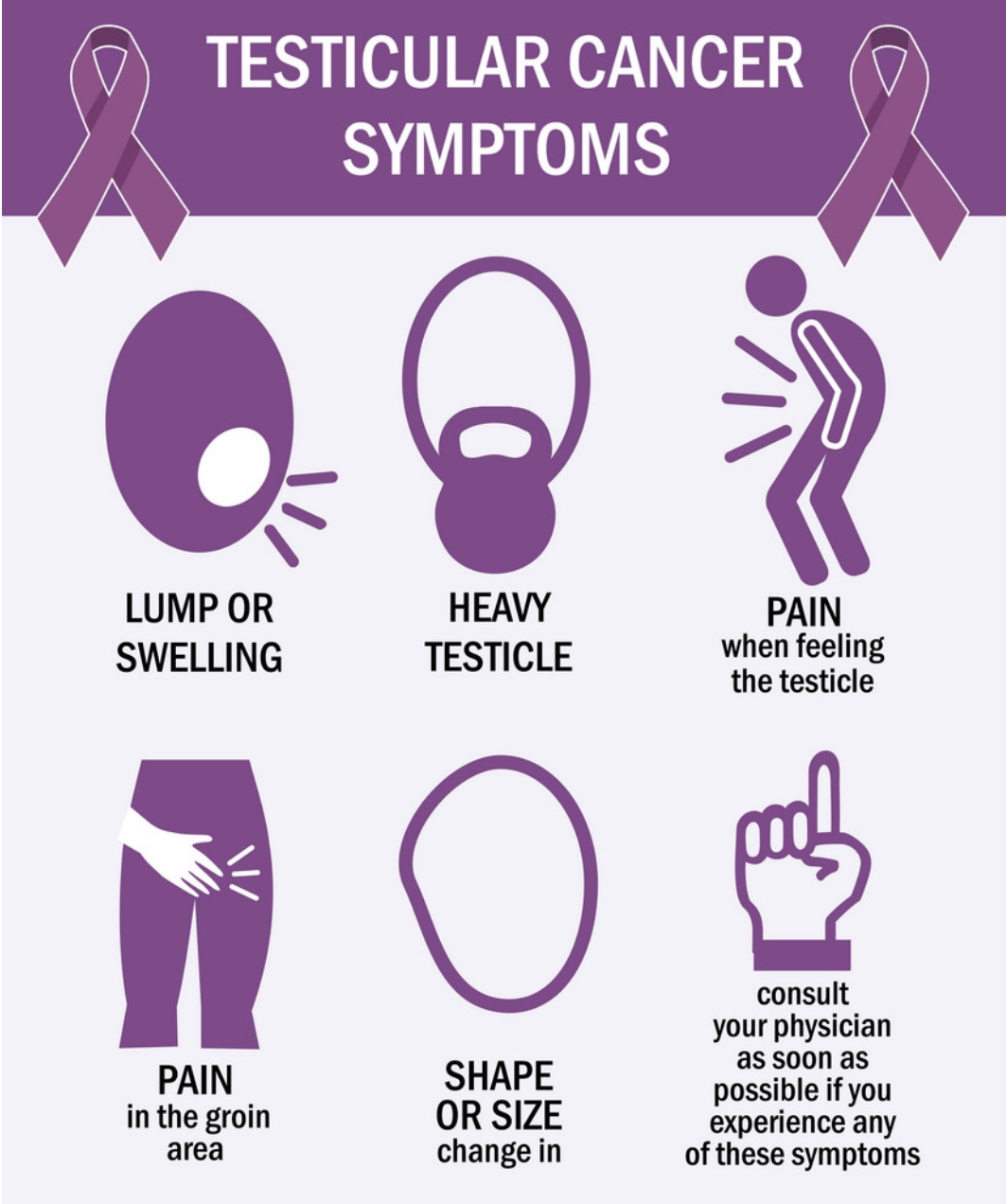
Testicular cancer mostly presents itself in the form of a lump. There may be no pain in these lumps. However, there may be swelling. Only a third of the patients complain about dull pain. The following are the few symptoms that patients of the testicular cancer experience.
- The patient may report a difference in how they feel their testicles.
- There may be a presence of faint pain in the lower abdomen. The patient can also feel this type of pain in the groin regions.
- There may be a build-up of fluid in the scrotum.
- Patients may report an uncomfortable feeling in testicles or scrotum.
- Metastasis of testicular cancer can cause systemic effects. This usually depends on the part of the body where cancer has spread.
Causes of Testicular cancer
Like the majority of the cancers, the leading cause of testicular cancer is not clear. Some of the doctors predict that it may be because of alteration in the testicles at the cellular level. A healthy set of cells grow and divide properly. However, certain abnormalities can affect cellular growth. This results in the division of the cells even without the body needs them. Accumulation of these abnormal cells results in the formation of tumors in testicles. Almost all of the cells begin due to abnormality in germ cells. The reason for the development of normal germ cells into abnormal ones is not clear.
DIAGNOSIS
The majority of the lumps present in the scrotum are non-cancerous. However, it is important that the doctor asses the tumours. An early diagnosis helps in the development of an effective strategy.
Physical Examination
The doctor can physically examine the scrotum. Further imaging tests will be ordered to check out
Scrotal Ultrasound
After an initial diagnosis, the doctor will suggest a scrotal ultrasound. Other than the scrotal ultrasound, HRCT helps in obtaining the imaging of testicles.
Tumour Biomarkers
Three serum tumour markers may be present in patients who have testicular cancers. These tumor biomarkers are
- Alpha Fetoprotein
- Beta unit of human chorionic gonadotropin
- Lactate Dehydrogenase
Elevation of AFP and Beta-HCG occurs in 80% of the patients.
Staging
After the diagnosis of testicular cancer, certain tests help to find out the stage of cancer. Stages of testicular cancer are follows
Stage 0
The other name for this stage is Testicular Intraepithelial Neoplasia. In this stage, the cancerous cells are present in the tiny tubules. This is the same area wherein the sperms develop. Tumour marker levels in this stage are normal.
Stage I
There are two subtypes of stage I testicular cancer. Determination of subtype of stage I depends on the inguinal orchiectomy. In stage IA, cancer spread to the inner layers of testicles and epididymis. In stage IB, cancer has spread to the blood or lymph vessels. It also includes the spermatic cord, scrotum, or the outer layer of the testicular membrane.
Stage II
Stage II testicular cancer has three subtypes. Stage IIIA exists around the testicles, spermatic cord, and the scrotum. This stage has invaded about 5 lymph nodes and is larger than 2cm in size. Stage IIB has spread to more than 5 lymph nodes. Stage IIC is larger than five centimeters in size. In all subtypes of stage II, the tumour marker may be normal or slightly higher than normal.
Stage III
Stage III also has three subtypes, similar to Stage II. Stage IIIA exists in the testicles, spermatic cord, and/or scrotum. It has spread some of the lymph nodes in the abdomen. The cancerous cells have spread to the distant lymph nodes or the lungs. Stage IIIB is different from Stage IIIA because one or more of the tumour markers may be above normal. Stage IIIC has high levels of one or more tumour biomarkers.
Treatment of Testicular Cancer
Treatment strategies for testicular cancer depend on the staging of cancer. The following are certain treatment options for patients of testicular cancer.
Surgery
Surgery involves the removal of the testicles. The name for this procedure is inguinal orchiectomy. The doctor may also remove some of the lymph nodes that cancer has spread to.
Radiation Therapy
This treatment involves high energy X-rays. It may be external or internal radiation therapy. External radiation focuses on the X-rays outside the body. Internal radiation uses radioactive substances present in the needles, catheters, and others.
Chemotherapy
Chemotherapy is the administration of special drugs—these drugs aid in stopping the division of the cancer cells. The doctor may inject these drugs systematically.
High Dose Chemotherapy with a combination of stem cell transplant
This treatment is suitable for those testicular cancers that have metastasized. Stem cell replacement helps in stopping the formation of cancerous cells.
REFERENCES